GP Fellowships and Mentoring - £10000 a year?
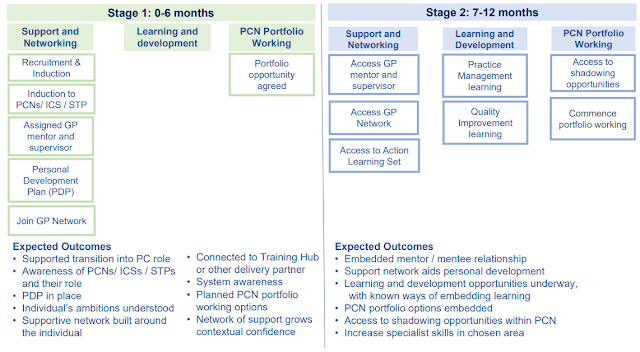
Details have come out about a new fellowship scheme which will be available to all newly qualified GPs (and nurses) working in Primary Care. It will be offered to all newly qualified GPs in a fellowship scheme which will provide at least 1 hour of mentor-ship every 4 weeks and at least 6 sessions of coaching over the 2 years. Locums cannot apply, it is aimed for salaried GPs though partners can apply. It is also offered to nurses interested in primary care but I will not cover that here. You would sign up to a 2 year scheme and participants receive funded mentor-ship and funded CPD opportunities of one session per week (pro rata), and rotational placements within or across PCNs to develop experience and support transition into the workforce. To allow this to happen, the NHS will pay £10,200 to the practice to release their GP fellow out for a session a week for their CPD and also mentor-ship. Over the 2 years, it will form a sort of curriculum which I assume will mak...