GP Stories - Free lunch
On Disney+, there is currently a great dramatisation of the opiate epidemic that started in America called Dopesick. It explains the unscrupulous methods that this pharmaceutical company used to market their drug Oxycontin to physicians: nice meals out, filling up their fuel tanks, trips to Florida to listen to pain lectures. It shows the devastation that uncontrolled opiate prescribing can do to patients and seemingly to those around them. In this country, we do get drug reps around here but they don't seem to have as much power to do that sort of thing here. When in hospital, I remember the makers of Vesicare took the urology team out for a curry one evening, and our consultant gave us a talk on the drug. It clearly had an effect, as I remember it clearly and it is front of mind for overactive bladder. In primary care, its more limited to 'educational lunches', the big companies bring M&S and waitrose food, smaller companies bring in tesco meal deals - definitely not as memorable. Compared to America, UK doctors are more bound to stricter prescribing guidelines, some drugs aren't licenced on NICE or you would have to go off guidelines which has more risks to the prescribing doctor. So maybe that's why they don't invest as much into the persuading the UK doctors to prescribe their drug.
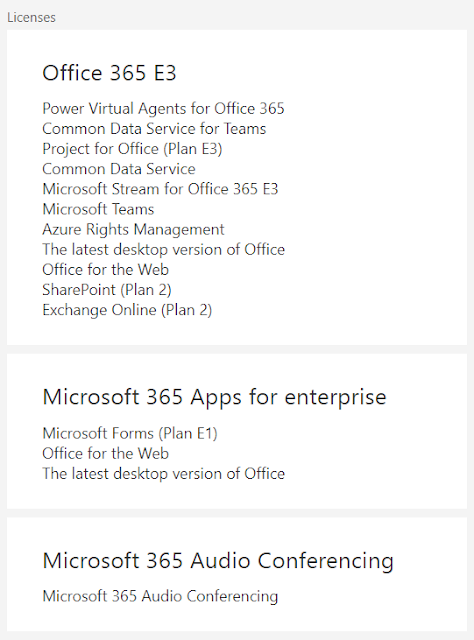
 |
| 10mg Oxycontin pill |
Opiates and many other drugs are addictive, and it is invariably so hard to try to get people off them once they are hooked and dependant. It is the staple of the duty GPs urgent list that there will be some patient who needs a top up of their painkiller / anxiety medication / sleeping tablet. Now there will be some with genuinely need it, but there will be a significant few that either are constantly forgetting it on the bus or ending up doubling their dose so they've run out too soon. We have patients that are on 2-day repeat scripts of their medications to prevent them overusing it - it just puts extra strain on the pharmacy to refill their script and a bit more time for the doctor to prescribe it that regularly. Some of these patients have been doing this regime for decades.
The 'resilient' thing (the buzz word for GPs) would be to straight up refuse the prescription and that should hopefully educate the patient that they should stick to the dose as prescribed so they won't run out, and also that they can survive without the medication in the first place. However, in a large team of clinicians, it would only take one doctor who would be considered 'softer' who would in theory undermine the resilience of the rest. Also with patient demand reaching all time highs and doctor staffing levels becoming lower and lower, maybe the easiest and quickest thing would be to sign that script. Weaning patients that have been on these medication for years takes a lot of time, time that GPs don't have. With waiting times for operations such as knee and hip replacements increasing, it is likely that requests for these medications will just increase, and if we just refuse them, they end up calling 111 or attending A+E for their fix. No easy solutions for this tough problem.

Comments
Post a Comment