New GP Contract Sparks Controversy and Anger
The recent unveiling of the revised GP contract by NHS England has sent shockwaves through the healthcare community, igniting a fierce debate. While some elements of the contract have garnered cautious acceptance, the British Medical Association's General Practitioners Committee (BMA GPC) has expressed strong disapproval of several key points, raising concerns about the potential impact on patient care, workload management, and the overall sustainability of primary care.
A Funding Landscape, Falling Short of Expectations:
The new contract offers a 2.23% funding uplift, a figure that fails to meet the BMA GPC's request of 4.17%. This shortfall, they argue, falls significantly short of what's needed to address the escalating pressures of inflation and ongoing staff shortages within the already under-resourced GP sector. This lack of sufficient funding, the BMA warns, risks further exacerbating existing difficulties faced by GP practices, potentially compromising patient care in the long run.
Beyond the Funding Figure: A Multifaceted Landscape of Discontent:
While the funding increase is a primary point of contention, the BMA GPC outlines several additional areas of concern:
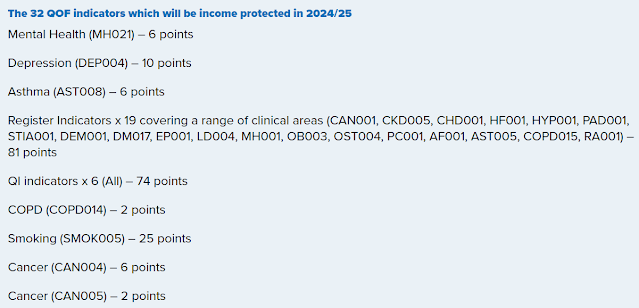
Quality and Outcomes Framework (QOF) Reduction: The proposed reduction in the number of protected QOF indicators has raised alarm bells. These indicators, vital for driving patient-centred care by incentivizing preventative measures and chronic disease management, may be de-emphasized under the new contract. 32 QOF indicators will be income protected for the 2024/2025 year, using points scored from the previous year. The QOF indicators are below, these total 212 points:
Funding Formula Concerns: The BMA raises anxieties about potential inequities arising from changes to the funding formula, which could disproportionately affect practices in deprived areas, leading to disparities in resources and service delivery. This could widen existing health inequalities and further disadvantage those who most need accessible and high-quality healthcare.
Workload Management Concerns: The proposed workload management strategies are met with scepticism, with the BMA questioning their effectiveness in addressing the already-existing pressures of staff shortages and high patient demand.
Digitalization: While acknowledging the potential benefits of digitalization, the BMA highlights the need for a clear and well-developed implementation plan. This plan should ensure adequate support for both practices and patients, particularly those who may lack access to technology or require additional assistance navigating the digital healthcare landscape. This would mitigate potential disruptions to care and bridge the digital divide, ensuring equitable access to healthcare services for all.
Seeking Solutions Through Referendum and Potential Industrial Action
The BMA is taking a two-pronged approach in response to the concerns surrounding the contract:
- National Referendum: A nationwide referendum amongst GP members will gauge their collective stance on the new contract. The outcome will significantly influence the BMA's future course of action and act as a clear indicator of the depth and breadth of GP dissatisfaction.
- Possible Industrial Action: The BMA has not ruled out the possibility of resorting to industrial action, which could involve work stoppages or other forms of protest. However, this depends on the referendum's outcome and the level of GP support for such measures.
The new GP contract has undoubtedly ignited controversy, highlighting the complex challenges faced within the primary care sector. While NHS England aims to implement changes, the BMA GPC raises valid concerns about the potential impact on patient care, working conditions, and resource allocation. Moving forward, open communication and collaboration between NHS England and the BMA are crucial to finding a solution that addresses the needs of GPs, patients, and the healthcare system as a whole. By working together, they can ensure a sustainable and high-quality future for general practice in England, one that prioritizes both patient well-being and the well-being of the healthcare workforce they rely on.
Please share below

Comments
Post a Comment